- SIWI – Leading expert in water governance
- /
- Latest
- /
- What does water have to do with antimicrobial resistance?
What does water have to do with antimicrobial resistance?
The World Antibiotic Awareness Week (18-24 November) draws attention to a global challenge that still seems to fly under the radar of many decision-makers. But projections estimate an annual death toll of 10 Million people globally by 2050 due to infections that have become resistant to treatment. In this blog post, Nicolai Schaaf explains why this is a water challenge and how SIWI is working to solve it.
The key drivers of antimicrobial resistance (AMR) are irresponsible use, environmental pollution and the lack of new, effective antibiotics. The lack of new substances is a market and regulation failure that requires massive investments in research and development, as well as new business models for the pharmaceutical industry. But water plays a crucial role in the context of both usage and pollution.
Access to safe water, sanitation and hygiene (WASH) is one of the most important containment factors for infectious diseases. Especially vulnerable groups like children are exposed to resistant infections, but often lack access to WASH. As long as we use antibiotics in this sense as a substitute for safe water, we will not solve the AMR problem. Adequate WASH infrastructure and governance from the megacities to the remotest regions is a health imperative, not only in the context of AMR.
In addition, antibiotics must be used wisely so that they can work better when needed. Antibiotics can treat bacterial infections, not viral infections like a common cold. Still, many people see antibiotics as a universal medicine and expect to receive antibiotics for all kinds of diseases. Instead, a proper diagnosis and targeted treatment are most important. And since most antibiotics and other pharmaceuticals are excreted after usage, it also puts a responsibility on wastewater treatment plants to adequately treat these substances. Today, this is a rare exception.
Responsible usage of antibiotics is even more important for animal health and food production, where antibiotics are used in vast amounts not only for treating sick animals but also for prevention and growth promotion of entire stocks. The case of aquaculture illustrates drastically how this practice impacts aquatic ecosystems and serves as a breeding ground for resistant microorganisms. But also in pork, cattle and poultry farming, irresponsible use of antibiotics is common throughout the world. There is even growing concern over antibiotics usage for crops.
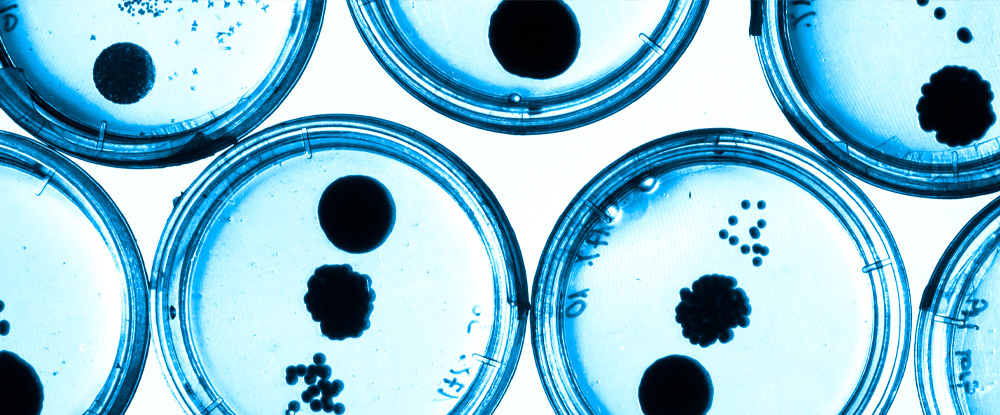
Through all these practices, antibiotics get in contact with microorganisms and water. If the concentrations are high enough, this can trigger resistance genes. Once this has happened, the risk of transfer to other places and to pathogens becomes just a matter of time. SIWI is therefore currently developing projects targeting tools for WASH and AMR in healthcare facilities and sustainable use of antibiotics in aquaculture.
Another environment where antibiotics concentrations can be dangerously high is in the effluent of antibiotics manufacturing sites with insufficient waste or wastewater treatment. SIWI engages with antibiotics suppliers, regulators and public procurers to improve the sustainability in the antibiotics supply chains as well as the global demand for sustainably produced antibiotics.
In sum, water is one of the key vectors for antibiotic pollution, pathogens and resistance genes. Responsible manufacturing, usage and management of antibiotics must go hand in hand with waste and effluent management. The global activities during World Antibiotic Awareness Week will highlight critical topics like access to medicine and better usage and hopefully even prevention, including the role of WASH. But systematic monitoring and regulation of maximum concentrations in waterbodies are lacking throughout the world and it will be hard to achieve and measure progress if we do not fully acknowledge the role of water in the fight against AMR.
Most recent

SIWI Amman and UNICEF host Libya representatives for WASH exposure visit
- Water, Sanitation and Hygiene (WASH)
- Water governance

Water and land: Partners in climate mitigation
- Water in landscapes
- Wetlands
- Water governance

What is the role of water in rural and urban school facilities?
- Water, Sanitation and Hygiene (WASH)
- Water in landscapes
- Water governance
- Gender and water

Taking root: locally driven forest landscape restoration
- Water in landscapes
- Wetlands
- Groundwater
- Resilience through water

Realising rights through safe sanitation

Water fundamental to a healthy planet and people

6 reasons the world needs more responsibly manufactured antibiotics
